Skin Cancer
Skin cancer
- Skin cancer is a malignant growth on the skin which can have many causes. The three most common skin cancers are basal cell cancer, squamous cell cancer, and melanoma, each of which is named after the type of skin cell from which it arises. Skin cancer generally develops in the epidermis (the outermost layer of skin), so a tumor is usually clearly visible. This makes most skin cancers detectable in the early stages. Unlike many other cancers, including those originating in the lung, pancreas, and stomach, only a small minority of those afflicted will actually die of the disease. Skin cancer represents the most commonly diagnosed cancer, surpassing lung, breasts, colorectal and prostate cancer. Melanoma is less common than basal cell carcinoma and squamous cell carcinoma, but it is the most serious—for example, in the UK there are 9,500 new cases of melanoma each year, and 2,300 deaths. It is the most common cancer in the young population (20 – 39 age group). It is estimated that approximately 85% of cases are caused by long periods of exposure to the sun. Non-melanoma skin cancers are the most common skin cancers, and the majority of these are basal cell carcinomas. These are usually localized growths caused by excessive cumulative exposure to the sun and do not tend to spread.
Signs and symptoms
-
There are a variety of different skin cancer symptoms. These include changes in the skin that do not heal, ulcering in the skin, discolored skin, and changes in existing moles, such as jagged edges to the mole and enlargement of the mole.
> Basal cell carcinoma usually looks like a raised, smooth, pearly bump on the sun-exposed skin of the head, neck or shoulders. Sometimes small blood vessels can be seen within the tumor. Crusting and bleeding in the center of the tumor frequently develops. It is often mistaken for a sore that does not heal. This form of skin cancer is the least deadly and with proper treatment can be completely eliminated, often without scarring.
> Squamous cell carcinoma is commonly a red, scaling, thickened patch on sun-exposed skin. Ulceration and bleeding may occur. When SCC is not treated, it may develop into a large mass. Squamous cell is the second most common skin cancer. It is dangerous, but not nearly as dangerous as a melanoma.
> Most melanomas are brown to black looking lesions. Warning signs that might indicate a malignant melanoma include change in size, shape, color or elevation of a mole. Other signs are the appearance of a new mole during adulthood or new pain, itching, ulceration or bleeding.
> Merkel cell carcinomas are most often rapidly growing, non-tender red, purple or skin colored bumps that are not painful or itchy. They may be mistaken for a cyst or other type of cancer.
Causes
-
Skin cancer has many potential causes, these include:
>Studies have shown that smoking tobacco and related products can double the risk of skin cancer.
>Overexposure to UV-radiation may cause skin cancer either via the direct DNA damage or via the indirect DNA damage mechanism. Overexposure (burning) UVA & UVB have both been implicated in causing DNA damage resulting in cancer. Sun strength between 10AM and 4PM is most intense. Natural (sun) & artificial UV exposure (tanning salons) are possibly associated with skin cancer.
> UVB rays primarily affect the epidermis causing sunburns, redness, and blistering of the skin when overexposed. The melanin of the epidermis is activated with UVB just as with UVA; however, the effects are longer lasting with pigmentation continuing over 24 hours.
> Chronic non-healing wounds, especially burns. These are called Marjolin’s ulcers based on their appearance, and can develop into squamous cell carcinoma.
> Genetic predisposition, including “Congenital Melanocytic Nevi Syndrome”. CMNS is characterized by the presence of “nevi” or moles of varying size that either appear at or within 6 months of birth. Nevi larger than 20 mm (3/4″) in size are at higher risk for becoming cancerous.
> Human papilloma virus (HPV) is often associated with squamous cell carcinoma of the genitals, anus, mouth, pharynx, and fingers. It is believed that the HPV vaccine might help to prevent these cancers as well as cervical cancers.
> Skin cancer is one of the potential dangers of ultraviolet germicidal irradiation.
> Deficiencies in certain vitamins and minerals.
Prevention
-
Although it is impossible to completely eliminate the possibility of skin cancer, the risk of developing such a cancer can be reduced significantly with the following steps:
> Avoid the use of tobacco products.
> Reducing overexposure to ultraviolet (UV) radiation, especially in early years
> Avoiding sun exposure during the peak UV times during the day, typically from 10 AM to 3 PM (dependent on country) when the sun is directly over head
> Wearing protective clothing (long sleeves and hats) when outdoors
> Using a broad-spectrum sunscreen that blocks both UVA and UVB radiation
> Reapply sun block as per the manufacturers directions
> Ensuring suitable unprotected exposure (15 minutes a day suggested maximum) to the sun to allow adequate Vitamin D formation. - Australian scientist Ian Frazer who developed a vaccine for cervical cancer, says that a vaccine effective in preventing for certain types of skin cancer has proven effective on animals and could be available within a decade. The vaccine would only be effective against Squamous Cell Carcinoma.
Pathology
-
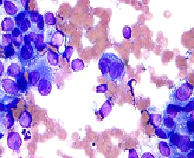
Micrograph of melanoma. FNA specimen. Field stain.
Squamous cell carcinoma is a malignant epithelial tumor which originates in epidermis, squamous mucosa or areas of squamous metaplasia.Macroscopically, the tumor is often elevated, fungating, or may be ulcerated with irregular borders. Microscopically, tumor cells destroy the basement membrane and form sheets or compact masses which invade the subjacent connective tissue (dermis). In well differentiated carcinomas, tumor cells are pleomorphic/atypical, but resembling normal keratinocytes from prickle layer (large, polygonal, with abundant eosinophilic (pink) cytoplasm and central nucleus). Their disposal tends to be similar to that of normal epidermis: immature/basal cells at the periphery, becoming more mature to the centre of the tumor masses. Tumor cells transform into keratinized squamous cells and form round nodules with concentric, laminated layers, called “cell nests” or “epithelial/keratinous pearls”. The surrounding stroma is reduced and contains inflammatory infiltrate (lymphocytes). Poorly differentiated squamous carcinomas contain more pleomorphic cells and no keratinization.
Treatment
- Treatment is dependent on type of cancer, location of the cancer, age of the patient, and if the cancer is primary or recurrence. One should look at the specific type of skin cancer (basal cell carcinoma, squamous cell carcinoma, or melanoma) of concern in order to determine the correct treatment required. An example would be a small basal cell cancer on the cheek of a young man, where the treatment with the best cure rate (Mohs surgery) might be indicated. In the case of an elderly frail man with multiple complicating medical problems, a difficult to excise basal cell cancer of the nose might warrant radiation therapy (slightly lower cure rate) or no treatment at all. Topical chemotherapy might be indicated for large superficial basal cell carcinoma for good cosmetic outcome, whereas it might be inadequate for invasive nodular basal cell carcinoma or invasive squamous cell carcinoma.[citation needed]
- For low-risk disease, radiation therapy (external beam radiotherapy or brachytherapy), topical chemotherapy (imiquimod or 5-fluorouracil) and cryotherapy (freezing the cancer off) can provide adequate control of the disease; both, however, may have lower overall cure rates than certain type of surgery. Other modalities of treatment such as photodynamic therapy, topical chemotherapy, electrodessication and curettage can be found in the discussions of basal cell carcinoma and squamous cell carcinoma.
- Mohs’ micrographic surgery (mohs surgery) is a technique used to remove the cancer with the least amount of surrounding tissue and the edges are checked immediately to see if tumor is found. This provides the opportunity to remove the least amount of tissue and provide the best cosmetically favorable results. This is especially important for areas where excess skin is limited, such as the face. Cure rates are equivalent to wide excision. Special training is required to perform this technique.
- Scientists have recently been conducting experiments on what they have termed “immune- priming”. This therapy is still in its infancy but has been shown to effectively attack foreign threats like viruses and also latch onto and attack skin cancers. More recently researchers have focused their efforts on strengthening the body’s own naturally produced “helper T cells” that identify and lock onto cancer cells and help guide the killer cells to the cancer. Researchers infused patients with roughly 5 billion of the helper T cells without any harsh drugs or chemotherapy. This type of treatment if shown to be effective has no side effects and could change the way cancer patients are treated.
 Emergency Help line
Emergency Help line 
