Lung Cancer
Lung cancer
-
Lung cancer is a disease of uncontrolled cell growth in tissues of the lung. This growth may lead to metastasis, which is the invasion of adjacent tissue and infiltration beyond the lungs. The vast majority of primary lung cancers are carcinomas of the lung, derived from epithelial cells. Lung cancer, the most common cause of cancer-related death in men and women, is responsible for 1.3 million deaths worldwide annually. The most common symptoms are shortness of breath, coughing (including coughing up blood), and weight loss.
The main types of lung cancer are small cell lung carcinoma and non-small cell lung carcinoma. This distinction is important, because the treatment varies; non-small cell lung carcinoma (NSCLC) is sometimes treated with surgery, while small cell lung carcinoma (SCLC) usually responds better to chemotherapy and radiation. The most common cause of lung cancer is long-term exposure to tobacco smoke. The occurrence of lung cancer in nonsmokers, who account for as many as 15% of cases, is often attributed to a combination of genetic factors, radon gas, asbestos, and air pollution, including secondhand smoke.
Signs and symptoms
-
Symptoms that suggest lung cancer include:
> dyspnea (shortness of breath)
> hemoptysis (coughing up blood)
> chronic coughing or change in regular coughing pattern
> wheezing
> chest pain or pain in the abdomen
> cachexia (weight loss), fatigue, and loss of appetite
> dysphonia (hoarse voice)
> clubbing of the fingernails (uncommon)
> dysphagia (difficulty swallowing).
Causes
- The main causes of lung cancer (and cancer in general) include carcinogens (such as those in tobacco smoke), ionizing radiation, and viral infection. This exposure causes cumulative changes to the DNA in the tissue lining the bronchi of the lungs (the bronchial epithelium). As more tissue becomes damaged, eventually a cancer develops.
-
Smoking
Smoking, particularly of cigarettes, is by far the main contributor to lung cancer. Across the developed world, almost 90% of lung cancer deaths are caused by smoking. In the United States, smoking is estimated to account for 87% of lung cancer cases (90% in men and 85% in women). Among male smokers, the lifetime risk of developing lung cancer is 17.2%; among female smokers, the risk is 11.6%. This risk is significantly lower in nonsmokers: 1.3% in men and 1.4% in women. Cigarette smoke contains over 60 known carcinogens, including radioisotopes from the radon decay sequence, nitrosamine, and benzopyrene. Additionally, nicotine appears to depress the immune response to malignant growths in exposed tissue.
-
Radon gas
Radon is a colorless and odorless gas generated by the breakdown of radioactive radium, which in turn is the decay product of uranium, found in the Earth’s crust. The radiation decay products ionize genetic material, causing mutations that sometimes turn cancerous. Radon exposure is the second major cause of lung cancer, after smoking. Radon gas levels vary by locality and the composition of the underlying soil and rocks. For example, in areas such as Cornwall in the UK (which has granite as substrata), radon gas is a major problem, and buildings have to be force-ventilated with fans to lower radon gas concentrations. The United States Environmental Protection Agency (EPA) estimates that one in 15 homes in the U.S. has radon levels above the recommended guideline of 4 picocuries per liter (pCi/L) (148 Bq/m³). Iowa has the highest average radon concentration in the United States; studies performed there have demonstrated a 50% increased lung cancer risk, with prolonged radon exposure above the EPA’s action level of 4 pCi/L.
-
Viruses
Viruses are known to cause lung cancer in animals, and recent evidence suggests similar potential in humans. Implicated viruses include human papillomavirus, JC virus, simian virus 40 (SV40), BK virus, and cytomegalovirus. These viruses may affect the cell cycle and inhibit apoptosis, allowing uncontrolled cell division.
-
Asbestos
Asbestos can cause a variety of lung diseases, including lung cancer. There is a synergistic effect between tobacco smoking and asbestos in the formation of lung cancer. In the UK, asbestos accounts for 2–3% of male lung cancer deaths. Asbestos can also cause cancer of the pleura, called mesothelioma (which is different from lung cancer).
Diagnosis
-
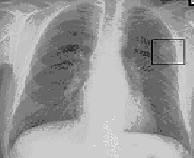
Chest radiograph showing a cancerous tumor in the left lung.
Performing a chest radiograph is the first step if a patient reports symptoms that may be suggestive of lung cancer. This may reveal an obvious mass, widening of the mediastinum (suggestive of spread to lymph nodes there), atelectasis (collapse), consolidation (pneumonia), or pleural effusion. If there are no radiographic findings but the suspicion is high (such as a heavy smoker with blood-stained sputum), bronchoscopy and/or a CT scan may provide the necessary information. Bronchoscopy or CT-guided biopsy is often used to identify the tumor type.
Abnormal findings in cells (“atypia”) in sputum are associated with an increased risk of lung cancer. Sputum cytologic examination combined with other screening examinations may have a role in the early detection of lung cancer.
-
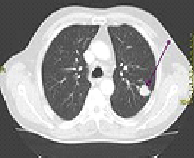
CT scan showing a cancerous tumor in the left lung.
The differential diagnosis for patients who present with abnormalities on chest radiograph includes lung cancer as well as nonmalignant diseases. These include infectious causes such as tuberculosis or pneumonia, or inflammatory conditions such as sarcoidosis. These diseases can result in mediastinal lymphadenopathy or lung nodules, and sometimes mimic lung cancers. Lung cancer can also be an incidental finding: a solitary pulmonary nodule (also called a coin lesion) on a chest radiograph or CT scan taken for an unrelated reason.
Staging
- Lung cancer staging is an assessment of the degree of spread of the cancer from its original source. It is an important factor affecting the prognosis and potential treatment of lung cancer. Non-small cell lung carcinoma is staged from IA (“one A”; best prognosis) to IV (“four”; worst prognosis). Small cell lung carcinoma is classified as limited stage if it is confined to one half of the chest and within the scope of a single radiotherapy field; otherwise, it is extensive stage.
Treatment
-
Surgery
If investigations confirm lung cancer, CT scan and often positron emission tomography (PET) are used to determine whether the disease is localized and amenable to surgery or whether it has spread to the point where it cannot be cured surgically.
Blood tests and spirometry (lung function testing) are also necessary to assess whether the patient is well enough to be operated on. If spirometry reveals poor respiratory reserve (often due to chronic obstructive pulmonary disease), surgery may be contraindicated.
Surgery itself has an operative death rate of about 4.4%, depending on the patient’s lung function and other risk factors. Surgery is usually only an option in non-small cell lung carcinoma limited to one lung, up to stage IIIA. This is assessed with medical imaging (computed tomography, positron emission tomography). A sufficient preoperative respiratory reserve must be present to allow adequate lung function after the tissue is removed.
Procedures include wedge resection (removal of part of a lobe), segmentectomy (removal of an anatomic division of a particular lobe of the lung), lobectomy (one lobe), bilobectomy (two lobes), or pneumonectomy (whole lung). In patients with adequate respiratory reserve, lobectomy is the preferred option, as this minimizes the chance of local recurrence. If the patient does not have enough functional lung for this, wedge resection may be performed. Radioactive iodine brachytherapy at the margins of wedge excision may reduce recurrence to that of lobectomy.
Video-assisted thoracoscopic surgery and VATS lobectomy have allowed for minimally invasive approaches to lung cancer surgery that may have the advantages of quicker recovery, shorter hospital stay and diminished hospital costs.
-
Radiotherapy
Radiotherapy is often given together with chemotherapy, and may be used with curative intent in patients with non-small cell lung carcinoma who are not eligible for surgery. This form of high intensity radiotherapy is called radical radiotherapy. A refinement of this technique is continuous hyperfractionated accelerated radiotherapy (CHART), in which a high dose of radiotherapy is given in a short time period. For small cell lung carcinoma cases that are potentially curable, chest radiation is often recommended in addition to chemotherapy. The use of adjuvant thoracic radiotherapy following curative intent surgery for non-small cell lung carcinoma is not well established and is controversial. Benefits, if any, may only be limited to those in whom the tumor has spread to the mediastinal lymph nodes.
-
Prognosis
Prognostic factors in non-small cell lung cancer include presence or absence of pulmonary symptoms, tumor size, cell type (histology), degree of spread (stage) and metastases to multiple lymph nodes, and vascular invasion. For patients with inoperable disease, prognosis is adversely affected by poor performance status and weight loss of more than 10%. Prognostic factors in small-cell lung cancer include performance status, gender, stage of disease, and involvement of the central nervous system or liver at the time of diagnosis.
-
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy). When chemotherapy is placed directly into the spinal column, an organ, or a body cavity such as the abdomen, the drugs mainly affect cancer cells in those areas (regional chemotherapy). Bladder cancer may be treated with intravesical (into the bladder through a tube inserted into the urethra) chemotherapy. The way the chemotherapy is given depends on the type and stage of the cancer being treated.
-
Adjuvant chemotherapy for NSCLC
Adjuvant chemotherapy refers to the use of chemotherapy after surgery to improve the outcome. During surgery, samples are taken from the lymph nodes. If these samples contain cancer, the patient has stage II or III disease. In this situation, adjuvant chemotherapy may improve survival by up to 15%. Standard practice is to offer platinum-based chemotherapy (including either cisplatin or carboplatin).
Adjuvant chemotherapy for patients with stage IB cancer is controversial, as clinical trials have not clearly demonstrated a survival benefit. Trials of preoperative chemotherapy (neoadjuvant chemotherapy) in resectable non-small cell lung carcinoma have been inconclusive.
 Emergency Help line
Emergency Help line 
