Renal (Kidney) Cancer
Renal cell carcinoma
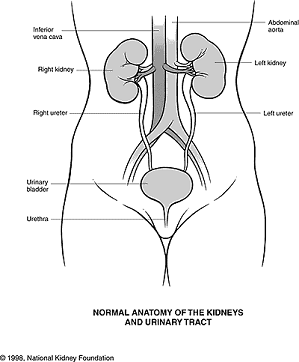
- Renal cell carcinoma (RCC, also known as hypernephroma) is a kidney cancer that originates in the lining of the proximal convoluted tubule, the very small tubes in the kidney that filter the blood and remove waste products. RCC is the most common type of kidney cancer in adults, responsible for approximately 80% of cases. It is also known to be the most lethal of all the genitourinary tumors. Initial treatment is most commonly a radical or partial nephrectomy and remains the mainstay of curative treatment. Where the tumour is confined to the renal parenchyma, the 5-year survival rate is 60-70%, but this is lowered considerably where metastases have spread. It is resistant to radiation therapy and chemotherapy, although some cases respond to immunotherapy. Targeted cancer therapies such as sunitinib, temsirolimus, bevacizumab, interferon-alpha, and possibly sorafenib have improved the outlook for RCC (progression-free survival), although they have not yet demonstrated improved survival.
Signs and symptoms
-
The classic triad is hematuria (blood in the urine), flank pain and an abdominal mass. This triad only occurs in 10-15% of cases, and is generally indicative of more advanced disease. Today, the majority of renal tumors are asymptomatic and are detected incidentally on imaging, usually for an unrelated cause.
Signs may include:
> Abnormal urine color (dark, rusty, or brown) due to blood in the urine (found in 60% of cases)
> Loin pain (found in 40% of cases)
> Abdominal mass (25% of cases)
> Malaise, weight loss or anorexia (30% of cases)
> Polycythemia (5% of cases)
> Anaemia resulting from depression of erythropoietin (5% of cases)
> The presenting symptom may be due to metastatic disease, such as a pathologic fracture of the hip due to a metastasis to the bone
> Varicocele, the enlargement of one testicle, usually on the left (2% of cases). This is due to blockage of the left testicular vein by tumor invasion of the left renal vein; this typically does not occur on the right as the right gonadal vein drains directly into the inferior vena cava.
> Vision abnormalities
> Pallor or plethora
> Hirsutism – Excessive hair growth (females)
> Constipation
> Hypertension (high blood pressure) resulting from secretion of renin by the tumour (30% of cases)
> Elevated calcium levels (Hypercalcemia)
> Paraneoplastic disease
> Night Sweats
v
> Severe Weight Loss
Classification
-
Recent genetic studies have altered the approaches used in classifying renal cell carcinoma. The following system can be used to classify these tumors:
> Clear cell carcinoma (VHL and others on chromosome 3)
> Papillary carcinoma (MET, PRCC)
> Chromophobe renal carcinoma
> Collecting duct carcinoma -
Risk factors
Cigarette smoking and obesity are the strongest risk factors. Hypertension and a family history of the disease are also risk factors.
Dialysis patients with acquired cystic disease of the kidney showed a 30 times greater risk than in the general population for developing RCC.
Exposure to asbestos, polycyclic aromatic hydrocarbons, gasoline has not been shown to be consistently associated with RCC risk.
Diagnosis
-
By Signs and symptoms But unfortunately, early kidney cancers do not usually cause any signs or symptoms, but larger ones may.
Anamnesis (detailed medical review of past health state)
Physical examination A physical exam can provide information about signs of kidney cancer and other health problems. The doctor checks general signs of health and tests for fever and high blood pressure. and the doctor may be able to feel an abnormal mass when he or she examines your abdomen.
If a patient has symptoms that suggest kidney cancer, the doctor may perform one or more of the following procedures:
Lab tests Lab tests are not usually used to diagnose kidney cancer, but they can sometimes give the first hint that there may be a kidney problem. They are also done to get a sense of a person’s overall health and to help tell if cancer may have spread to other areas. They can help tell if a person is healthy enough to have an operation.
Urinalysis(Urine tests) These set of tests check for several indicators of the cancer such as blood, sugar, proteins, and bacteria.
Complete blood count A complete blood count can detect findings sometimes seen with renal cell cancer.Blood chemistry tests Blood chemistry tests are usually done in people who may have kidney cancer, as it can affect the levels of certain chemicals in the blood.
-
Bone scan
Biopsy Biopsies are not often used to diagnose kidney tumors. Imaging studies usually provide enough information. But, biopsy is sometimes used to get a small sample of cells from a suspicious area if imaging test results are not conclusive enough to warrant removing a kidney. Biopsy may also be done to confirm the diagnosis of cancer if a person’s health is too poor for surgery and other local treatments (such as radiofrequency ablation, arterial embolization or cryotherapy) are being considered. (10 questions to ask your doctor before a Biopsy)
Pathology
Gross examination shows a yellowish, multilobulated tumor in the renal cortex, which frequently contains zones of necrosis, hemorrhage and scarring.
Light microscopy shows tumor cells forming cords, papillae, tubules or nests, and are atypical, polygonal and large. Because these cells accumulate glycogen and lipids, their cytoplasm appear “clear”, lipid-laden, the nuclei remain in the middle of the cells, and the cellular membrane is evident. Some cells may be smaller, with eosinophilic cytoplasm, resembling normal tubular cells. The stroma is reduced, but well vascularized. The tumor compresses the surrounding parenchyma, producing a pseudocapsule.
Radiology
The characteristic appearance of renal cell carcinoma (RCC) is a solid renal lesion which disturbs the renal contour. It will frequently have an irregular or lobulated margin. Traditonally 85 to 90%% of solid renal masses will turn out to be RCC but this number may be decreasing as renal masses are being found at smaller and smaller sizes with larger numbers of benign lesions. 10% of RCC will contain calcifications, and some contain macroscopic fat (likely due to invasion and encasement of the perirenal fat). Following intravenous contrast administration (computed tomography or magnetic resonance imaging), enhancement will be noted, and will highlight the tumor relative to normal renal parenchyma.
Treatment
-
Surgery
Micrograph of embolic material in a kidney removed because of renal cell carcinoma (cancer not shown). H&E stain.
Surgical removal of all or part of the kidney (nephrectomy) is recommended. This may include removal of the adrenal gland, retroperitoneal lymph nodes, and possibly tissues involved by direct extension (invasion) of the tumor into the surrounding tissues. In cases where the tumor has spread into the renal vein, inferior vena cava, and possibly the right atrium, this portion of the tumor can be surgically removed, as well. In cases of known metastases, surgical resection of the kidney (“cytoreductive nephrectomy”) may improve survival, as well as resection of a solitary metastatic lesion. Kidneys are sometimes embolized prior to surgery to minimize blood loss. -
Percutaneous therapies
Percutaneous, image-guided therapies, usually managed by radiologists, are being offered to patients with localized tumor, but who are not good candidates for a surgical procedure. This sort of procedure involves placing a probe through the skin and into the tumor using real-time imaging of both the probe tip and the tumor by computed tomography, ultrasound, or even magnetic resonance imaging guidance, and then destroying the tumor with heat (radiofrequency ablation) or cold (cryotherapy). These modalities are at a disadvantage compared to traditional surgery in that pathologic confirmation of complete tumor destruction is not possible. Therefore, long-term follow-up is crucial to assess completeness of tumour ablation.
-
Medications
RCC “elicits an immune response, which occasionally results in dramatic spontaneous remissions.” This has encouraged a strategy of using immunomodulating therapies, such as cancer vaccines and interleukin-2 (IL-2), to reproduce this response. IL-2 has produced “durable remissions” in a small number of patients, but with substantial toxicity. Another strategy is to restore the function of the VHL gene, which is to destroy proteins that promote inappropriate vascularization. Bevacizumab, an antibody to VEGF, has significantly prolonged time to progression, but phase 3 trials have not been published. Sunitinib (Sutent), sorafenib (Nexavar), and temsirolimus, which are small-molecule inhibitors of proteins, have been approved by the U.S. F.D.A.
-
Chemotherapy
Most of the currently available cytostatics are ineffective for the treatment of RCC. Their use can not be recommended for the treatment of patients with metastasized RCC,as response rates are very low,often just 5-15%,and most responses are short lived. The use of Tyrosine Kinase (TK) inhibitors, such as Sunitinib and Sorafenib, and Temsirolimus are described in a different section -
Vaccine
Cancer vaccines, such as TroVax, have shown promising results in phase 2 trials for treatment of renal cell carcinoma. However, issues of tumor immunosuppression and lack of identified tumor-associated antigens must be addressed before vaccine therapy can be applied successfully in advanced renal cell cancer.
 Emergency Help line
Emergency Help line 
